2376-0249
Clinical Image - International Journal of Clinical & Medical Images (2017) Volume 4, Issue 3
Author(s): Sharma BB, Dewan S, Bhardwaj N, Aziz MR
Introduction: Achilles tendon is very important tendon which connects the calf muscles to the heel bone. This is mainly responsible for the plantar flexion. This can rupture or torn which may be complete or incomplete. The rupture is more commonly noticed between third to fifth decades of life. The incidence is I in 15000 of general population and is doubled in active athlets. Male to female ratio is around 20:1 and majority occur by trauma.Ambroise Pare described the complete tear first time in 1575.
Case Report: A 63-years old diabetic female reported to the orthopedic department as she had twisted her right foot accidentally. In addition to that she had complaints of pain and difficult movements of two months duration. She is on ant diabetic treatment for the last two years, She had also had taken the course of ciprofloxacin for ten days because of some respiratory infection three months back and the details are not known. On examination she is slightly on obese side with slight difficulty in walking. Blood pressure revealed 144 mm of Hg systolic and 92 mm of Hg diastolic. Systemic examination was grossly normal.
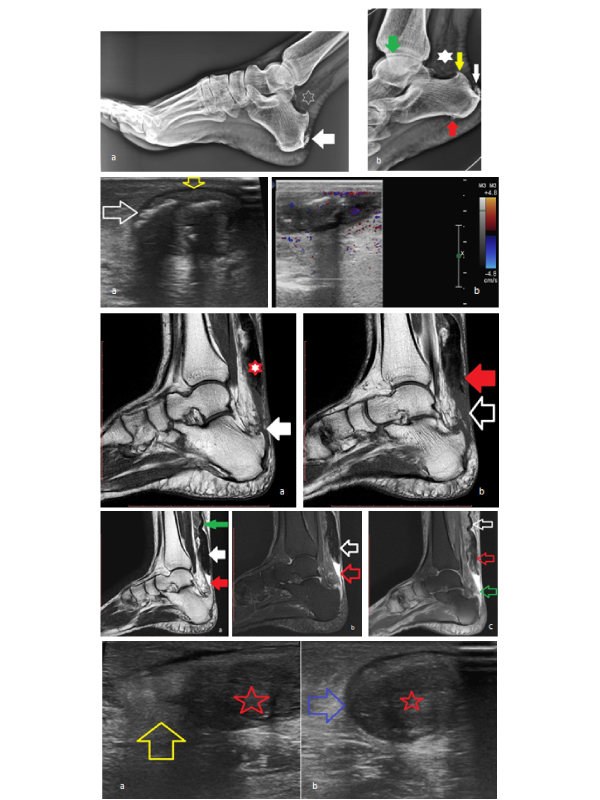
Locally the left foot had swelling on the posterior side of the heel. Thompson’s squeeze test was positive. There was no local bruise or ulceration. All the blood investigations were within normal limits. Random blood sugar and haemoglobin were 110 mg/dl and 11 g/dl respectively. Plain X-ray of the left foot revealed obliteration of Kager’s triangle and calcification of the insertional end of the Achillis tendon (Figure 1a and 1b).
Ultrasound examination had revealed the torn tendon with well defined sheath outline. The torn tendon was visualized with fluid collection (Figure 2a and 2b). Color doppler study did not reveal any vascularity in the torn tendinous fibers (Figure 3a and 3b). The patient was subjected to magnetic resonance imaging of left foot with leg to evaluate the achills tendon morphology in relation to bones and joints (Figures 4-6). C) Proton density (PD) spectral attenuated inversion recovery (SPAIR) image shows crumpled tendon (white arrow) with ruptured tendon end and fluid in the emptied space (green arrow) Patient had been advised for debridement and tendon transfer in the tertiary hospital.
Discussion: Sports related injuries are responsible for various injuries to Achilles tendon. Achilles is one of the strongest tendons of the body and measures about 15 cm connecting three muscles (gastrocnemus, soleus and plantaris) to the calcaneum (Figure 7). This receives blood supply from musculo-tendinous junction and nerve supply from sural and tibial nerves. This muscle helps in walking, running and jumping by strong contraction. Two most common pathologies of this tendon are: tendinopathy and tear or rupture. The inflammation of the tendon can either be at non insertional part or insertional part. The former is seen more common in young and active people and the later in middle aged and elderly individuals. The main cause of the tear or rupture is trauma which can cause mild to severe injury. There can be micro tears and interstitial tears which are parallel to the muscle fibres.Repeated traumas can lead to these injuries which can become chronic in nature with duration of more than four weeks. Platt mentioned that untreated rupture may lead to adherence of tendinous sheath to the underlying torn tendon. This will further makes the movements difficult and surgical interventions are not smooth. Many factors other than trauma are also responsible for this entity like rheumatoid arthritis, diabetes mellitus, gout and SLE, local steroid injection, medication of steroids and quinoline antibiotics (ciprofloxacin and oflaxacin). The commonest site is proximal to the insertion which is quite hypo vascular in nature [1]. The rupture can easily be diagnosed by clinical Thompson’s or Simmonds squeeze test. There is palpable gap in the lower end of the tendon near insertion with decreased plantar flexion and increased passive dorsiflexion. The rupture of Achilles tendon had been classified by Kuwada[2] as follow:
type i - less than 50% rupture and treated with cast immobilization
type ii - complete rupture with gap <3 cm
type iii - complete rupture with gap 3-6 cm
type iv - when tendinous gap is >6 cm
type iii and type iv requires graft repair but type ii is treated with end to end anastomosis. Type i is treated conservatively [3,4].
Lateral plain X-ray of ankle shows obliteration of Kager’s triangle which is pre-achilles fat pad.thios can also shows any calcaneal aavulsion.there can be calcification of insertion end because of the chronicity. Ultrasonography is done with high frequency 7.5 MHz linear array probe. This modality is inexpensive and repeatable. Partial tear shows the hypoechoic or anechoic nature of the tendon along with >1 cm thickness of the tendon whereas full thickness shows torn ends with dirty shadowing [5,6]. MRI is required to categorize the rupture for the purpose of management.MRI can depict better tissue characterization. Normal tendon shows low intensity in all the sequences. Ruptured tendon shows increased thickness with gap filled up with either fluid or blood T2W shows increased intensity with >7 mm antero-posterior thickness. Ruptured tendon can be visualized within the tendinous sheath [7,8]. Management depends upon the type and grading of injury. Gastrocnemus recession is undertaken in non-ruptured tendon. RICE is indicated in mild cases. Debridement and repair is advised where tear is less than 50%. Debridement and tendon transfer in other cases where damage is more than 50% [9,10].
 Awards Nomination
Awards Nomination

