2376-0249
Clinical-Medical Image - International Journal of Clinical & Medical Images (2023) Volume 10, Issue 4
Author(s): Saadoune Mohamed*, Ibrahima Kalil Cisse, Darfaoui Mouna, Elomrani Abdelhamid and Khouchani Mouna
Department of Radiology, Mohammed VI University Hospital, Marrkech, Morocco
*Corresponding Author:
Saadoune Mohamed
Department of Radiology
Mohammed VI University Hospital
Marrkech, Morocco
Tel: +212 676579947
E-mail: Simoja151206@gmail.com; mohamed.saadoune@edu.uca.ac.ma
Received: 03 April 2023, Manuscript No. ijcmi-23-94290; Editor assigned: 05 April 2023, Pre QC No. P-94290; Reviewed: 17 April 2023, QC No. Q-94290; Revised: 22 April 2023, Manuscript No. R-94290; Published: 30 April 2023, DOI:10.4172/2376-0249.1000890
Citation: Mohamed S, Cisse IK, Mouna D, Abdelhamid E and Mouna K. (2023) Burkit’s Lymphoma of the Oral Cavity Revealed by a Rapidly Progressive Mega Mass in a Young Woman. Int J Clin Med Imaging 10:890.
Copyright: © 2023 Mohamed S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
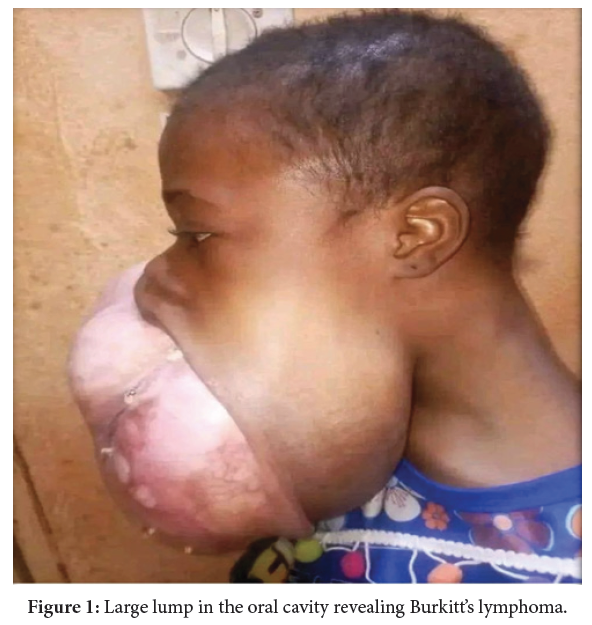
Burkitt’s lymphoma (LB) is a malignant tumor characterized by the proliferation of type B lymphoid cells. It is a non-Hodgkin’s lymphoma with a high degree of aggressiveness with significant tumor dissemination, in particular towards the bone marrow and the central nervous system. It represents 30 to 40% of non-Hodgkin’s lymphoma (NHL) in children [1,2]. In the equatorial regions, it represents 50% of childhood cancers and more than 70% of NHLs [3]. The prognosis of this tumor has improved considerably in recent years thanks to intensive and short therapeutic protocols, particularly in developing countries. We present the case of a young femal who presented with LB in the oral cavity (Figure 1).
Staging should be expedited because the tumor is growing rapidly. Staging uses fluorodeoxyglucose (FDG)-(PET) positron emission tomography/ CT; if not available, CT of the chest, abdomen and pelvis can be done instead. Patients should also undergo bone marrow biopsy, cerebrospinal fluid cytology and laboratory studies that include LDH (lactate dehydrogenase).
Treatment must be initiated quickly because these tumors grow rapidly. Intensive alternating polychemotherapy of cyclophosphamide, vincristine, doxorubicin, methotrexate, ifosfamide, etoposide, cytarabine (CODOX-M/IVAC) plus rituximab gives a cure rate > 80% in children and adults < 60 years. For patients > 60, regimens such as rituximab plus etoposide, prednisone, vincristine (Oncovin) and doxorubicin (at adjusted R-EPOCH doses) are also commonly used with success. In patients without CNS metastases, CNS prophylaxis (eg, with systemic and/ or intrathecal methotrexate and/or cytarabine) is essential.
Tumor lysis syndrome is common during treatment and patients should receive IV hydration, allopurinol often with rasburicase and urine alkalinization (in the absence of hyperphosphatemia), combined with close monitoring of the ionogram (in particular potassium, phosphorus and calcium). Rasburicase is contraindicated in G6PD deficiency because it may cause hemolytic anemia in these patients. Some patients may require dialysis for hyperkalemia.
Burkitt’s lymphoma; Oral localization; Diagnosis
The authors declare that they have no ties of interest.
[1] Satishchandra H, Sridhar AS and Pooja BP. (2013). Imaging of Burkitt's lymphoma-abdominal manifestations. J Cancer Res Ther 9: 128-130.
Google Scholar, Crossref, Indexed at
[2] Madani A, Benhmiddoune L, Zafad S, Harif MH and Quessar A, et al. (2005). Treatment of Burkitt's lymphoma in children using the LMB89 protocol in Casablanca. Cancer Lett 92: 193-198.
[3] Patil K, Mahima VG, Jayanth B S and Ambika L. (2007). Burkitt's lymphoma in an Indian girl: A case report. J Indian Soc Pedod Prev Dent 25: 194-199.
 Awards Nomination
Awards Nomination

