2376-0249
Clinical Image - International Journal of Clinical & Medical Images (2016) Volume 3, Issue 7
Author(s): Kiran S, Abhinav Jain, Deepak Gupta, Dhiraj Agarwal and Akash Shukla
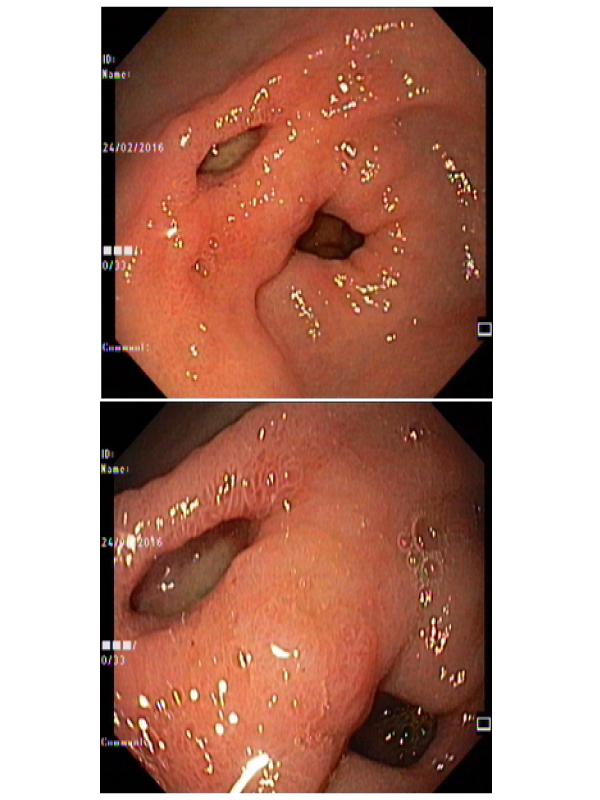
A 62-year old man, who was newly diagnosed as a case of cryptogenic cirrhosis, underwent screening esophago-gastro-duodenum (OGD) scopy for varices; he had no previous history of hepatic decompensation, upper gastrointestinal symptoms, other comorbidities, prolonged drug or alcohol intake. On physical examination, vital signs were stable and moderate ascites was detected. There were two openings noted in the gastric antrum, one of them was true pylorus and the other was a fistula (Figure 1a).The OGD scopy also showed small esophageal varices and mild portal hypertensive gastropathy seen as snake-skin appearance of the gastric mucosa surrounding the two openings (Figure 1b). The OGD scope could be passed into the duodenum through the pylorus but not from the fistulous tract. There was no evidence of peptic ulceration or scarring between the two openings.
Double pylorus (DP) is a rare finding reported in 0.06%-0.4% of upper gastrointestinal endoscopies, [1] characterized by the presence of two openings from the gastric antrum to the duodenal bulb, which may be congenital or acquired. The fistula remained open in the majority of patients (60%), converged with the normal pyloric ring in 25% of patients and disappeared in 5% on long term follow-up [2]. The most common cause of acquired DP is a benign gastric ulcer. [1] Other causes of acquired DP are malignant ulcers, systemic diseases such as diabetes mellitus, chronic renal failure, systemic lupus erythematous, etc. Also, prolonged intake of steroids, NSAID’S and alcohol may lead to fistula formation [1,3]. In congenital double pylorus, an error of canalization seems to occur [4]. In our case, possibility of a peptic etiology for the additional opening to the duodenum was more likely.
A biopsy was taken from the region between the two openings, which showed normal mucosa and a muscularis mucosae layer. Apart from a mild gastritis, no other pathology (chronic peptic ulcer, ulcerated malignancy) suggesting an acquired origin of the double pylorus was observed. Therefore, the case was considered to be congenital in origin. To our knowledge, only a few cases of DP in patients with liver diseases have been reported in the literature [5-7]. We report a unique case of congenital DP in a cirrhotic patient which is first of its kind to be reported.
 Awards Nomination
Awards Nomination

