2376-0249
Case Blog - International Journal of Clinical & Medical Images (2015) Volume 2, Issue 10
Author(s): Muhammad Imran Butt*
A 73-year-old- gentleman admitted to hospital for evaluation of gradual functional and cognitive decline over past 6 months. He had history of traumatic brain injury at age of 9 when a heavy carton fell accidently on his head. Unfortunately, patient did not undergo any surgery as there was no advance Neurosurgery available those days. Limited history of the mechanism of injury was available from sister who was 4 years younger than patient. Patient sustained right sided hemiplegia requiring a walking stick for mobilisation and remained cognitively well. No previous scans were available.
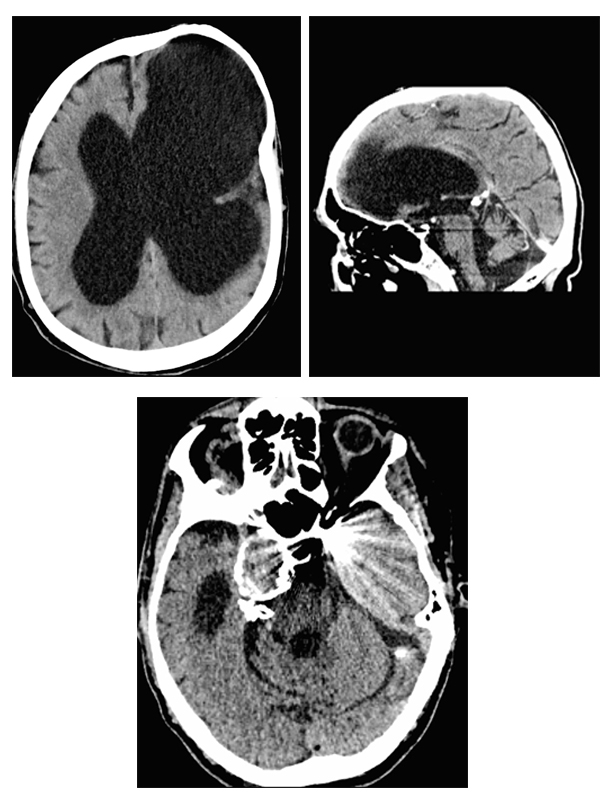
A CT angiogram was organised which revealed marked ex-vacuo dilatation of the left lateral ventricle with associated porencephalic cyst formation with chronic mass effect and mild right sided midline shift. Ventriculomegaly involving the right lateral, third and fourth ventricles was likely related to cerebral, cerebellar and brainstem volume loss. A giant aneurysm of right cavernous internal carotid artery (ICA) measuring 30 mm × 29 mm causing impression on the surrounding area was also seen. Adjacent to the left anterior clinoid process, a metallic fragment was noted - in absence of prior surgical/endovascular intervention, this was likely a post-traumatic fragment. The left internal carotid artery was completely occluded and there was no definite left anterior cerebral artery A1 segment evident. A neurosurgical opinion was sought to consider shunt for possible communicating hydrocephalus.
However, patient was deemed not suitable for surgery as patient`s cognitive decline was attributed to cerebrovascular disease rather than possible communicating hydrocephalus as well as likely poor outcome of surgery. Patient ended up in a high level of care nursing home. TBI has a wide range of presentation but a combination of large hydrocephalus, chronic thrombosis and ICA aneurysm with late cognitive decline is uncommon (Figures 1-3).
 Awards Nomination
Awards Nomination

